August 29, 2020
Two recent preprints* (here and here) suggest that herd immunity to COVID-19 is closer at hand than most of us, including myself, have thought, and that it has already been reached in New York City.
I am not an epidemiologist, so critiquing the formulas and methods in these papers is beyond my expertise. I therefore have reached out to interview the authors of these papers on my podcast, and I hope that they accept. Here is my attempt to explain the findings of these papers at a conceptual level.
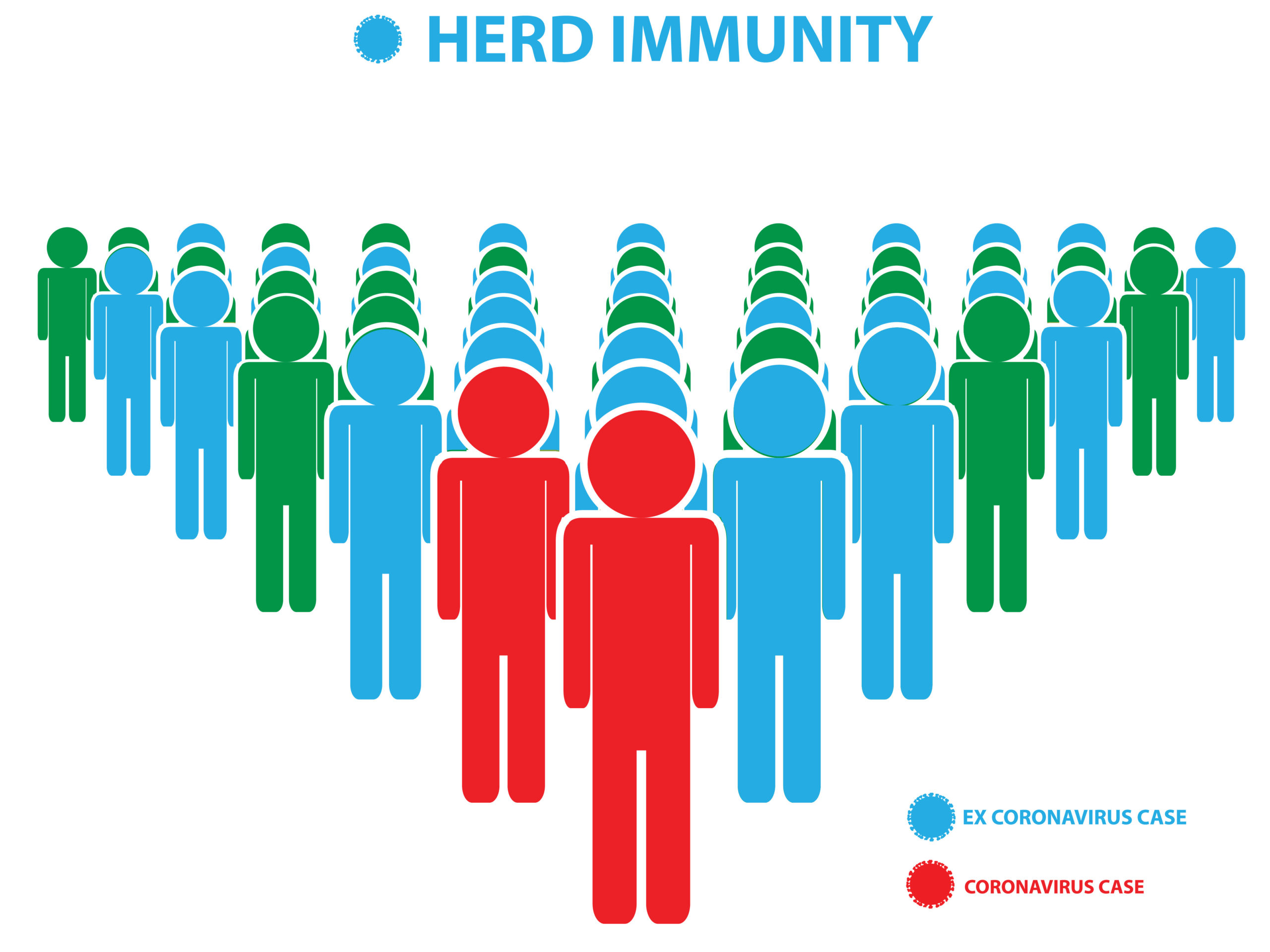
What Is Herd Immunity?
Herd immunity is the point at which enough people have either died or become immune that life can go on normally and each person who gets infected will, on average, transmit the disease to fewer than one other person. This results in a gradual decline of transmission that would have the potential to eventually lead to the disease's eradication, though eradication is not inevitable. So, herd immunity does not mean the end of the disease has come. It means that the numbers of new cases and deaths will decline over time rather than exponentially rising.
The number of people who need to be infected to reach herd immunity is the herd immunity threshold. This threshold is not the maximum number of people who can be infected. The threshold can be overshot for two reasons.
First, herd immunity does not automatically produce eradication, so people will continue to get infected after it is reached.
Second, at the beginning of the epidemic the disease can spread faster than immunity develops. While someone is sick, they are a vector of transmission. Only after they recover do they become immune and removed from the pool of transmitters. Since it takes a few weeks to acquire and recover from COVID-19, there would be a window a few weeks wide where rapid growth could overshoot the herd immunity threshold before the effect of that immunity kicks in.
Efforts to curb the rapid spread were referred to as flattening the curve in the early days of the epidemic, where the aim was to reduce the peak number of daily new hospitalizations to prevent the health care system from being overburdened.
Those same efforts, when applied in and around the reaching of the herd immunity threshold, would also be expected to prevent overshoot of that threshold, since the rate of growth surrounding the reaching of the threshold would be slower.
Calculating the Herd Immunity Threshold: The Standard Formula
What is that threshold?
The standard formula for the calculation of the herd immunity threshold is 1 – 1/R0. R0 (“R naught”) is the basic reproduction number, which is the number of people, on average, that would be infected by each person who becomes sick, assuming that 100% of people in the population are susceptible. This makes R0 a theoretical number that never actually applies, because it is never the case that all people within the population are equally susceptible. The actual number infected, on average, is Re, or the “effective reproduction number.” Nevertheless, the R0 can be inferred from the available data for the purposes of calculating the herd immunity threshold.
The higher the R0, the higher the herd immunity threshold. This is because 1/R0 becomes smaller, and thus the amount subtracted from 1 is smaller. If R0 is 2.5, the herd immunity threshold is 0.6, meaning 60% of the population has to be infected to reach herd immunity. If R0 is 5, the herd immunity threshold is 0.8, meaning 80% of the population has to be infected to reach herd immunity. This range of 60-80% is what has typically been reported as the threshold.
The Standard Formula Only Applies to Randomly Distributed Vaccines
As both papers we are discussing today point out, this formula only applies to randomly distributed vaccines.
The reason is that when vaccinations are randomly distributed, the people who are least likely to be transmitters of the disease are vaccinated just as often as the people who are most likely to transmit the disease.
In an epidemic that takes its natural course, by contrast, the virus very specifically infects the people that are most susceptible first. This removes all of the strongest vectors early on, and continues to selectively remove the vectors until the herd immunity threshold is reached.
Thus, in models designed for natural infections, the variability in susceptibility is a key determinant of the herd immunity threshold. If there is zero variability and everyone is equally susceptible, then the effective reproduction number equals the basic reproduction number, and the herd immunity threshold is the same as it would be for randomly distributed vaccinations. As long as the variability is non-zero, however, the herd immunity threshold is lower than it would be for randomly distributed vaccinations. If the variability is large, the threshold is much lower than it would be for randomly distributed vaccinations.
Is Europe Rapidly Approaching Herd Immunity?
The first paper we are discussing today came from researchers in the UK and Portugal. Their approach was to infer the variation in susceptibility from the observed patterns of growth. They calculated a coefficient of variation of susceptibility for each of several European countries. Abbreviated CV, this is the ratio of the standard deviation to the mean, and is a measure of how far the susceptibility of the bulk of the people within a society deviates from the average susceptibility.
A higher R0 leads to a higher threshold, while a higher CV leads to a lower threshold. When R0 is between 2.5 and 5, and when the CV is between 2 and 5, the herd immunity threshold ranges from 10% to 20%. When inferring these values from the patterns of the epidemic, the values depend on the assumptions they made about whether people randomly mix with each other, or primarily mix with people that have similar social connectivity to themselves. The first assumption led to a lower R0 and a higher CV, while the second assumption led to a higher R0 and a lower CV. The end result was that the herd immunity threshold stayed very similar.
The estimated thresholds for the countries they examined were 9.6-11% in Belgium, 20-21% in England, 6-7.3% in Portugal, and 11-12% in Spain.
They concluded, “In all four countries considered here we foresee [the herd immunity threshold] being achieved between July and October and the COVID-19 epidemic being mostly resolved by the end of 2020.”
Have New York City and Chicago Reached Herd Immunity?
The second paper came out of the University of Illinois at Urbana-Champaign, where I did my postdoc, with one researcher from the Brookhaven National Laboratory in Upton, NY. This appears to have been submitted to the Proceedings of the National Academy of the Sciences, a very prestigious journal, and probably under peer review there, since the manuscript is marked with “PNAS” in the footer.
Rather than inferring an all-encompassing CV to characterize the variation in susceptibility, they estimated its component parts, splitting it into variability in social behavior and variation in biological susceptibility. As a proxy for the variation in biological susceptibility, they substituted the variation in susceptibility between different age groups.
They noted that this could exaggerate the actual variation because more severe cases will be more commonly reported than less severe ones, leading to greater disparities in the reporting of cases between ages than in the actual occurrence of infections between cases. However, they also noted that it could underestimate the biological variability since many other factors besides age may impact it.
Personally, I suspect this is a rather dramatic underestimation of the true variability, since I believe genetics, metabolic health, and nutrition are all likely to have large effects that go even beyond the well characterized “preexisting conditions” and are mostly independent of age. Moreover, we already know that up to half the population has some degree of preexisting T cell immunity driven by exposure to animals and common cold viruses, though we don't know how strongly that protects against infection.
NYC Has Reached It; Chicago is Close
Nevertheless, their model predicts that New York City, with an infection rate close to 30%, has already reached herd immunity, while Chicago, with an infection rate only a little over 10%, has not.
The near-30% value for NYC is at least a slight overshoot of the herd immunity threshold, and possibly a large one. The paper estimates the threshold may begin with around 15% of the population infected. It is easy to see how NYC could have overshot the threshold given how rapid the spread was during the peak of the epidemic.
Will There Be a Second Wave?
Their data at the time of analysis went up through June 1, and they included predictions for NYC and Chicago through September in a “worst-case scenario” of a complete opening up of the economy with no measures to mitigate transmission. It is almost September and that hasn't happened yet, so we can't test whether their predictions came true.
However, we can discuss them as hypotheticals.
If the true variability in susceptibility is four times less than they estimate (extremely unlikely), they predicted under a complete opening up NYC would have a second wave peaking in late July with 36,000 deaths, and Chicago would have a second wave in the same time frame with 128,000 deaths. If the variation was 25% less than they estimate (plausible), NYC and Chicago would both have much smaller second waves with 5,000 deaths in NYC and 4300 deaths in Chicago. If the variability matches their estimate, NYC would not have a second wave and Chicago would have a very small one with 2000 deaths. If the variability is 25% higher than their estimate, neither city would have any second wave at all.
Their conclusion is incredibly provocative:
By considering the worst-case scenario of a full relaxation of any currently imposed mitigation, we find that the results of the heterogeneity-modified model significantly modify the results from the homogeneous mode. In particular, based on our estimate of the immunity factor, we expect virtually no second wave in NYC, indicating that the herd immunity has likely been achieved there. Chicago, on the other hand, has not passed the herd immunity threshold that we infer, but the effects of heterogeneity would still result in a substantial reduction of the magnitude of the second wave there, even under the worst-case scenario. This, in turn, suggests that the second wave can be completely eliminated in such medium-hit locations, if appropriate and economically mild mitigation measures are adopted, including e.g. mask wearing, contact tracing, and targeted limitation of potential super-spreading events, through limitations on indoor bars, dining and other venues.
That NYC could completely open up and experience no second wave demands attention from everyone involved in policy here, as it's clear that the mitigation strategies are terrible for mental health, social vibrancy, and economic strength, and can only be justified if fully opening up does indeed lead to a second wave of cases and deaths.
NYC still experiences 200-250 new cases per day, but only 2-8 deaths per day. While any loss of life for any reason is tragic, deaths reached just under 600 per day at the peak of the epidemic. The most recent statistics on total mortality in NYC are for 2017, and they suggest an average daily death rate of 147. COVID-19 has gone from increasing the total mortality rate at least 4-fold to comprising about 3% of the total mortality rate. It has effectively become insignificant.
I have personally experienced this living in a busy section of the city, as the ambulances driving by my apartment have decreased from a pervasive and all-encompassing presence to an occasional one.
We Still Need to Be Cautious
We should be cautious about assuming herd immunity for several reasons:
- Herd immunity doesn't stop new infections from happening altogether. The most vulnerable people and those in close contact to them will always need to take some level of precaution.
- We still don't know how long immunity lasts, and whether it is possible to get reinfected several months later.
- The virus could mutate, and that might allow it to reinfect people who are otherwise immune.
- If people respond to a full reopening up by compensating for the restrictions placed on them over the last year by engaging in much more frequent events involving large crowds than they otherwise would have during “normal life,” a large number of super-spreader events could alter the calculus of herd immunity and lead to dramatic “overshoot” of the threshold.
- While NYC has likely hit herd immunity, most other locations have not, and will be hitting it over the next few months.
Is Reinfection a Significant Threat?
If reinfection is a significant threat, there is no sign of it in NYC. NYC is not fully opened up, but it is far more open than it was during the peak of the epidemic, and the cases have been steadily decreasing since April 8. We are 4.5 months into this steady decline with no signs of reversal.
Still, we don't know how much the virus may mutate. The more it mutates, the more likely it is to become benign and coexist with us over the longhaul. Still, it could go the fate of the common cold, which is mainly a nuisance, or the fate of the flu, which has a considerable death toll among the most vulnerable each year. If the other coronaviruses that infect humans provide any clue, it would likely go the way of SARS (contained, virtually non-existent), MERS (100-500 cases per year globally), or the common cold (a widespread nuisance).
We Need a Robust Worldwide Discussion of This
Whether NYC has reached herd immunity, and whether most of Europe and the US is close to reaching it, demands a robust discussion on the global stage. While I believe that we should be cautious about opening up, doing so in 4-week phases to test whether case loads increase as a result, being at or close to the herd immunity threshold dramatically changes the calculus of how aggressive those phases should be. Opening up has its own promise to save lives, through improved mental health, reduced suicide and addiction, and robust economic productivity, which is needed to maintain the distribution food, basic necessities, and medical resources.
It also changes how we should be investing our research. If a vaccine is many more months out than herd immunity, we should be directing a much larger proportion of our research toward how to safely open up, how to prevent overshoot of the herd immunity threshold, and into programs to trace the evolution of the virus over time.
The researchers making these models should be given attention by local, state, and national governments, and get attention on the global stage, so that their contribution can inform policy.
The Bottom Line
NYC has probably hit herd immunity, while Chicago, most of the US, and most of Europe are likely to be close behind. The threshold required for herd immunity is much lower than commonly assumed, because natural infections selectively infect those most likely to transmit the disease, and the commonly stated thresholds are based on random vaccinations. Herd immunity does not mean infections stop. We still need to be cautious about how quickly we open up, and we still need to protect the most vulnerable. Nevertheless, that we are at or close to herd immunity needs to be given far more attention than it is, and needs to inform our policy going forward.
Stay safe and healthy,
Chris
Please Support This Service
Support the service by purchasing a copy of The Food and Supplement Guide for the Coronavirus.
Get the guide for free when pre-ordering my Vitamins and Minerals 101 book.
Or, you can offer support by buying Testing Nutritional Status: The Ultimate Cheat Sheet
Get the guide for free, get 30-50% off the pre-orders of my book, and get the Cheat Sheet for 50% off when you sign up for the CMJ Masterpass. Use the code COVID19 to save 10% off the membership price.
Here's a list of other ways to support my work: How You Can Support My Work
Discuss!
Here are three ways to discuss this topic, including asking me questions and getting a response:
- The Masterpass FREE Forum. This forum is free and open to anyone to participate. Anything related to health and nutrition, including all aspects of the coronavirus, is welcome. I will do my best to participate several times a week, though I expect this to eventually be very large and may at some point have to participate on a weekly basis if it starts to take on a life of its own.
- The Coronavirus Forum. This is for anyone who purchases The Food and Supplement Guide for the Coronavirus, pre-orders my upcoming Vitamins and Minerals 101 book, or joins the CMJ Masterpass (if you join, use the coupon code NEWSLETTER for 10% off the membership price). This forum is dedicated specifically to the coronavirus, has subsections based on topics (nutrition, medicine, lifestyle, mechanisms of disease), and has a section where the archive version of this newsletter is directly linked and each newsletter can be discussed as an individual thread. I consistently participate in this forum 3-5 times a week.
- The Masterpass Discussion Group. Preserved for those who join the CMJ Masterpass, it's the best place to ask me questions in a fairly intimate environment and get a rapid response. All topics I cover are fair game, and I consistently participate approximately five times per week. The Masterpass also has monthly live Zoom Q&As that are even more intimate.
Disclaimer
I am not a medical doctor and this is not medical advice. I have a PhD in Nutritional Sciences and my expertise is in conducting and interpreting research related to my field. Please consult your physician before doing anything for prevention or treatment of COVID-19, and please seek the help of a physician immediately if you believe you may have COVID-19.
Subscribe
If you aren't subscribed to the research updates, you can sign up here.
Archive
You can access an archive of these updates here.
*Footnotes
* The term “preprint” is often used in these updates. Preprints are studies destined for peer-reviewed journals that have yet to be peer-reviewed. Because COVID-19 is such a rapidly evolving disease and peer-review takes so long, most of the information circulating about the disease comes from preprints.