It may be, then, that an extreme imbalance between vitamins A and D leads to the synthesis of abnormally high amounts of MGP. If there is enough vitamin K to activate all of the MGP, it will help protect the soft tissues from calcification. If, instead, the vitamin K cannot keep up with the level of MGP being produced and the pool of vitamin K becomes depleted, soft tissue calcification ensues.
I further elaborated on this theory in my Spring, 2007 article “On the Trail of the Elusive X Factor: Vitamin K2 Revealed,” published in Wise Traditions, and in my December, 2007 hypothesis paper “Vitamin D Toxicity Redefined: Vitamin K and the Molecular Mechanism,” published in the peer-reviewed journal Medical Hypotheses.
That summer, when my hypothesis paper had been accepted but not yet published, I sent it to Drs. Xiang-Dong Wang and Heather Mernitz at Tufts University, who had just published a very interesting study showing the ability of an activated vitamin A derivative to protect against kidney stones caused by activated vitamin D without antagonizing its ability to protect against lung cancer. At the time, it looked like I was going to get into the program at Tufts and they were excited about carrying out an investigation with me of the vitamin K-dependent protein expression in the tissues preserved from their experiment. Things didn't work out at some level higher than the lab, so I never wound up being part of the Tufts program.
In 2008, Dr. Wang's laboratory apparently followed through on the investigation and collaborated with the laboratory of Dr. Sarah Booth, head of the biochemical and molecular nutrition program there and renowned vitamin K expert, to confirm my hypothesis. The resulting paper was pulished in the December, 2008 issue of the prestigious Journal of Nutrition.
In the two figures below, different letters above the bars indicate that the measurements represented by the bars are statistically significantly different from one another.
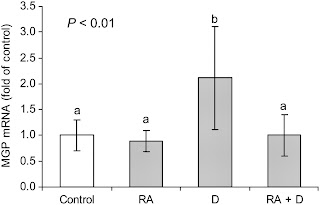
The above figure from the paper confirms the first part of the hypothesis: that vitamin D (the third bar) causes a large increase in the production of MGP in the kidney and that when vitamin A is added in combination with vitamin D (the fourth bar) it brings the production of this protein back down to normal.
If the production of vitamin K-dependent proteins such as MGP exceeds the capacity of the vitamin K pool or the enzyme that uses vitamin K, the vitamin K carboxylase, to activate them, these proteins will be produced in a defective state. At best, they will not protect against soft tissue calcification, and at worst, they could perhaps actively faciliate soft tissue calcification. The active form of MGP is called “carboyxlated MGP,” while the defective form is called “undercarboxylated MGP.”

In the above figure, part A shows the level of undercarboxylated, defective MGP; part B shows the level of carboxylated, active MPG; and part C shows the undercarboxylated-to-carboxylated MGP ratio, a lower ratio being better.
We can see a few important things here. First, activated vitamin D alone causes a marked increase in the defective form of MGP, and while activated vitamin A has no effect on the defective form alone, it brings the production of the defective form back down to normal when it is combined with activated vitamin D. Second, neither A nor D alone affect the production of the active form, but the two provided together synergistically increase the level of active MGP, which is what we want. Finally, we see that A improves the ratio all by itself, D dramatically worsens the ratio all by itself, and when the two vitamins are combined, they reduce the ratio with remarkable synergy.
Overall, then, we see that both vitamins are needed for optimal health. Vitamin A alone did nothing to benefit the kidneys or the lungs. Vitamin D alone caused a remarkable reduction in the ability of carcinogens associated with cigarette smoke to induce lung cancer but itself caused kidney stones. When vitamin A was combined with vitamin D, lung cancer was improved just as much, and the kidney calcification was completely eliminated. Moreover, the activation of vitamin K-dependent proteins in the kidney was much stronger with both vitamins than with neither treatment, suggesting that the vitamin A not only “antagonizes” vitamin D toxicity in the kidney, but that the two vitamins synergistically improve kidney health.
The authors made another interesting observation that I had not hypothesized: vitamins A and D appear to increase the turnover of vitamin K and the conversion of vitamin K1 to vitamin K2. In the D group, liver stores of K1 were reduced and kidney levels of MK-4, the form of vitamin K2 that animals synthesize, were increased. All A groups, whether the A was given alone or in combination with D, had reductions in both K1 and MK-4 levels. The authors referred to this as “antagonism” between vitamins A and K, but since vitamin A improved vitamin K-dependent activation of MGP, could it not be that the reduction in K1 was due to conversion of K1 to MK-4 and that the reduction in MK-4 was due to increased utilization and turnover of MK-4? The authors never suggested that vitamin D “antagonizes” vitamin K1, for example, even though its levels were reduced.
I have pointed out elsewhere that even modest amounts of vitamin D, whether provided by UV-light or in the diet, decrease liver stores of vitamin A; when the doses of D are larger, they decrease plasma levels of A as well. This suggests that vitamin D increases the need for and turnover of vitamin A. The data in the Tufts study suggest that vitamins D and A both increase the turnover of vitamin K2, but that vitamin A has a special effect of curbing the huge increase in the need for vitamin K2 in the kidney. Thus, vitamin A both calms the waves rocking the boat of vitamin D toxicity while helping to steer the ship at the same time, navigating the passengers to safety.
Is the theory that the fat-soluble vitamins “antagonize” one another rather than cooperate with one other ready to die the death it has long deserved? There is a reason, of course, that traditional diets and lifestyles provided all three of them together — because they cooperate with one another to support life, growth, and radiant health.
Update December 17, 2016: If you enjoyed this, I encourage you to check out The Ultimate Vitamin K2 Resource. It has easy-to-read practical advice, click-to-expand technical explanations, infographics that explain the science in a fun way, supplement recommendations, and a searchable database of foods. This post as well as the resource are indexed with my other vitamin K-related writings at Start Here for Vitamin K2.

[…] hypothesis, which has been confirmed by others, raises the possibility that the higher levels of 25(OH)D that were linked with lower bone density […]
[…] https://chrismasterjohnphd.com/2009/04/07/tufts-university-confirms-that-vitamin/?fbclid=IwAR2Izk2mj… […]
This blog is actually more interesting that i have thought of it before reading this awesome post.
Thank you for another great article.Trap
I started taking 4000 IU of Vitamin A in cod liver oil two years ago and find that my skin injuries heal faster. Its really interesting that adding Retinol both lowers MGP production which I had supposed but also improves carboxylation of MGP. This was unexpected and its why retinol is so successful at reducing calcium deposits since MGP is a central part of the calcium scavenging system. Normally the MK4 form of Vitamin K2 provides for carboxylation needs, but vitamin A must also be enhancing vitamin K2 production in the body. This observation files in the face of current medical advice that retinol should be avoided by people with bone loss. Japanese tests and research by Dr Vermeer in the Netherlands have shown MK4 to be very important and potent in reducing bone breakage rates and clearing calcium from soft tissues.
It seems that about 1.5 mg of MK4 vitamin K2 is needed in healthy older people to ensure carboxylation and thus healthy bones and calcium scavenging. For serious medical needs or those with fat absorption problems taking up to 5 mg two or three times a day works well. The Japan research was run with 15 mg of MK4 taken three times a day with a 30 mg good fat meal and 2000 IU of vitamin D, treatment worth considering for the most serious cases. American tests of MK4 run with only 200 iu of vitamin D and using BMD failed as MGP production was low with low D levels and MK4 acts on improving bone micro structure and connective tissues which are not observables in Dexa scans. Take away is that vitamin D boosts production of MGP and other carboxylation chemistry that are used to handle calcium placement or scavenging in the body, therefore requirements of MK4 go up especially in older adults and those with limited energy production like anorexics and marathon trainers.
I started on 1.3 mg of MK4 daily two years ago (Vitacost Ultra K with Advanced K2) and saw the gradual reduction in chest symptoms related to calcium load over several months. This was totally unexpected and nothing my three doctors were able to figure out or provide a solution for. Natto or MK7 is helpful but foreign to the body and has more side effects than MK4 which is made by all mammals. A good deal of the promotion for the MK7 vitamin K2 actually comes out of research on MK4 vitamin K2 where the reviewers conflated the two results to support MK7. In Japan its the MK4 form that is used in treatment since 1995 for bone loss and heart disease.
I often write on NOF.org as Tango02 on vitamin K2 for those wanting more information.
wondering if you had any comments on Bacillus subtilis? I have been hearing that it can be a major player in the intestinal bacteria by being co-factor with other beneficial microbiome bacteria. See :https://www.youtube.com/watch?v=MT6SdTUeJLc
Also – I make my own natto but do not like to eat soybeans. Is the MK-7 primarily in the slime on the beans? Can I swish the beans in warm water or broth and just drink this with a meal or add some palm oil (vit A) or codliver oil ( A and D)? You say MK-7 is sensitive to heat – is there a range like 110 to 140 degrees?
And finally – one of the main reasons I take MK-7 and MK-4 is to help dissolve osteocytes. I have a cervical spinal canal stenosis (congenital) and have already had a corpectomy to make more space. Sounds like MK-4 is very important for this process. Any sugestions on dosage and best sources?
Does heat degrade the k2 in natto?
I make natto using soybeans (have tried mung and black beans also) and do not seem to digest even fermented soybeans well.
My questions are:
Is most of the K2 on the slimy outer part of the soy bean and if so can warm/hot water be used to separate the slime from the bean and consume as a liquid?
Will this process leave a lot of K2 behind under the skin of the bean or inside the bean?
Autistic kids tend to suffer from an across-the-board deficiency of fat soluble vitamins. Vitamin A is important in helping to correct eye contact issues common with those on the spectrum, plus it helps in development of the immune system and mucosa lining of the stomach. Vitamin D is a great modulator of the immune system for these kids.
The question is – the traditional 4 to 1 or 8 to 1 ratio touted by the Weston Price foundation would seem to be "excessive". Am I off base when thinking a 2 to 1 ratio would be more applicable (say a 6 year old, 45 lbs – 1800 IU Vitamin A in the form of CLO and 900 IU Vitamin D)?
"A couple of months ago I started to supplement with cod liver oil, without a change to the D3 supplementation level. The result was that the serum level of 25OHD3 dropped by about 25%. Should I increase the D3 dosage to restore to 60 ng/ml?"
I know this was posted years ago, but if somehow you are still following this thread I'd like an update! I, too, found K2 decreased my D. I'm trying to figure out optimal levels (if I can get past the fact that I may be hypercalcemic). But you didn't say how much cod liver oil you were taking… so it's impossible for me to make an educated guess based on your experience. I cannot for the life of me find anyone on the internet reporting actual ratios *in their experience* as opposed to a seemingly random recommendation made by a salesman doctor like Dr. Mercola. I know that for me 100mcg MK-4 seems to be too much for 1000IU Vitamin D. Yet, this is supposedly a pretty tiny amount. Given that I am already D deficient or borderline deficient, among other things, the effect is pretty evident in taking even small doses of any supplements affecting calcium. My 100mcg MK-4+1000IU D supplement clearly deteriorated my oral hygiene quickly. I can't think of any other probably explanation for this other than that it was depleting my Vitamin D. Well… maybe I should've taken them with a meal containing moderate levels of calcium. Hmm. I'm scared to try things now given how much supplements have F'd up my body… every bloody one did opposite of what it was supposed to. But at some point soon I will probably give into temptation to test this out. Maybe wait for my test results first. If the doc recommends D, at least I have that excuse for trying more supplements even though I should've learned my lesson about them by now.
Go to inspire.com and you will reap tons on the D3-K2 stuff! Good people and studies!
Thanks for your work on this. Hmm. I believe K2 reduces my Vitamin D levels, while Vitamin D makes me hypercalcemic. So. I'm kind of screwed. But wondering what you think is the appropriate ratio of Vitamin A to Vitamin D. I have a supp 10k IU A + 400IU D, and that seems whack to me. I've read that 10k IU A is toxic if taken daily. Think I'll stick to my multivitamin.
I like this post, as well as this whole site. it is very well written and the info that you have presented here is also top tier and a great read for me. Please keep writing such excellent material. Thanks alot.
Chris, fascinating blogging. I regret to be jumping in the middle and don't know where to begin the VA/VD blog trail. Could you point me to the evidence that:
"even modest amounts of vitamin D, whether provided by UV-light or in the diet, decrease liver stores of vitamin A; when the doses of D are larger, they decrease plasma levels of A as well. This suggests that vitamin D increases the need for and turnover of vitamin A." Was this work in humans or what animal model? Plasma VA is so tightly regulated, I wonder… I was involved in some carotenoid and vitamin A research pursuing my PhD at UW Madison and am trying to figure this A and D balance thing out. Currently they are finding that vitamin A fortification of sugar in rural Africa has potentially increased liver stores of vitamin A to "sub-toxic" levels. Do you dispute the toxicity threshold of liver vitamin A as 1 umol/g? These rural kids probably do not get much vitamin D in their diets, but spend nearly all day outside. I'd like to take any discussion offline if you have the time. Regards!
Is there any information about this subject in other languages?
By which I mean, they make good use of retinol in their products at respectable doses for various indications and don't replace it with carotene.
Chris, last year the Clinicians supplement range in New Zealand brought out their "sunshine vitamin" product; each sublingual (sic) tablet contains D3 100O iu (25mcg), K2 (MK7) 90mcg.
They're a respected, research based concern that keep updating and reformulating their products, and I reckon they've been reading your blog. We'll know for sure when "sunshine vitamins" turns up with vitamin A in it. Some of their other products contain retinol.
Hi George,
Interesting, thanks!
Based on this photo I took I wonder if Vitamin Shoppe (major chain in the US) reads my stuff:
https://www.facebook.com/photo.php?fbid=494745773894389&set=pb.108150349220602.-2207520000.1370616947.&type=3&theater
Chris
I am a big fan of the subjects discussed. I also enjoy reading the comments, but notice that alot of people should stay on topic to try and add value to the original blog post.
Wow, this is confusing. I started taking a Vitamin D3 supplement last year when my level was diagnosed at 20 ng/ml. I took about 3000 IU per day for a 9 months and my level rose to 27 ng/ml.
Recently, I came across research that D3 supplementation, even in the 2000-3000 IUs a day dosage, without K2 supplementation will cause calcification of arteries and soft-tissues.
Wanted to ask the more knowledgeable in our community for input:
1) How much K2 and D3 should I take?
2) Is there a test to measure calcification and can it be reversed with K2 supplementation?
Thanks in advance!
GS
Hello, Mister Chris I am so confused and overwhelmed 🙁 Does this imply that D3 just cancels K2 out, or vice versa if you take them concurrently? I read one account saying they either have not had 25OHD increase or felt any change with regard to K benefits. Help :'(
Hi Chris. excellent information.
I've got several friends who are trying to get pregnant now, and are terrified of Vitamin A due to supposed birth defects. I was hoping you could direct me to some sources that would help counter their fears.
thanks,
dancinpete.
Chris, congratulations on being part of a really vital thread of scientific research that ordinary people around the world can benefit from in an immediate practical way! Truth is its own reward. It's great to see science and tradition merging in this kind of research. As you know, I've been following your work for quite a few years and I'm deeply grateful for it. Your work on vitamin A has given me a lot of confidence to eat traditional foods like liver despite all the fear-mongering about retinol and osteoporosis. After years of synthesizing information from many sources, I feel certain I'm following a path towards optimal health.
Having year-round access to UV B radiation was a major factor in my decision to move to Hawaii recently. These days I go out in the sun with just shorts for about 30 minutes (I have very light skin) around noon everyday to make vitamin D, and the cornerstone of my diet is eating fresh local grass-fed beef liver (about a pound per week, eaten raw) and local free-range chicken eggs with orange yolks (about three dozen per week, yolk only, eaten raw). I also eat about a pound per week of local grass-fed beef muscle meats, including heart, eaten raw as well. I get local fresh small-medium-size fish (e.g. opelu), which I get whole so I can eat the tiny little liver as a tasty fresh morsel, steam the fish, eat the flesh, and then simmer the carcass to make soup for the next meal. So I'm definitely getting large and BALANCED amounts of vitamins A, D and K2! Unfortunately I can't find a local source of tiny fish to eat for calcium, so I take a Ca + Mg supplement, and I also eat local fresh seaweed for minerals. Unfortunately it's very hard to find raw milk here (my favorite food–for years I drank a quart or two per day), but of course it's totally unnecessary so I don't dwell on it. I eat fresh coconut, fruit and veggies to round out my caloric needs.
My PUFA intake is very low across the board, but not low enough to be deficient because I get a tiny amount of omega-6 from macadamia nuts (about .2g omega-6 in a serving of a half-dozen kernels), a small amount of omega-6 and omega-3 from beef, a small amount of omega-3 from fish, and as much as several grams per day of omega-6 from avocado. Total PUFA works out to around 5g per day, about 2% of total caloric intake, with a 6:3 ratio of about 5:1.
Obviously I have no need for cod liver oil these days (I enjoyed consuming tiny amounts of it for several years in the past), but I've also changed my attitude towards it. I don't think I'd consume it even if I lived in an area with a vitamin D winter, because it makes more sense to me to eat fresh local liver (beef, chicken, fish, whatever) for the vitamin A, fresh local fish for the omega-3, and a vitamin D pill in variable amounts as a sensible compromise and adaptation to the arbitrary conditions of one's climatological and technological environment in the modern world. My reasoning is three-fold: you sidestep the quality control issues in the current CLO supply and the widespread use of fortification; you get the extra nutrients of eating whole foods; and you get to eat locally and sustainably instead of relying on one species of fish from a distant part of the world.
My story is similar to Chris. Believed all the hype of no red meat and lots of soy. Health deteriorated fast after an illness. Anxiety, joint pain, severe fatigue. I read Eat Fat, Lose Fat and then turned it all around.
I make an egg drink everyday with cinnamon, coconut oil, butter and I also add black strap molasses because it has lots of minerals. I also take High Vitamin Cod Liver Oil and a supplement with Hydroxyappetite Calcium, magnesium, vit K, vit D and other nutrients. This has completely taken care of the lack of energy that I had. I was thinking that if people are seeing a drop in Vitamin D levels from taking cod liver oil, they may have taken the ones that remove the vitamins.
Louise L
Chris–
Kinda sucks that the folks at Tufts didn’t even bother to include you as a co-author on that paper, when you are basically the one who proposed the experiment.
I mean, seriously.
At the very least, they could have kept you in the loop as to what was happening.
Something’s not right there.
-Greg
Chris,
Thanks for the post. Can you mention the ratio of Vitamin A and D?
I intend taking Vitamin D 5000 IU per day.
Venkat
Great blog. I'm convinced that there is benefit going from 45 ng/ml to 60 ng/ml 25-hydroxy D test, and am willing to consider going higher if evidence bears that out.
See this chart for expected disease prevention rates as a function of vitamin D level:
https://www.imminst.org/forum/index.php?act=attach&type=post&id=6065
In a 3-year Japanese osteoporosis study, 15 mg of K2-MK4 was given to Japanese women three times a day without any adverse reactions (PMID 17287908).
So, here's my oil soluble vitamin intake:
vitamin D: 7500 IU (gives me 62 ng/ml)
vitamin A: 10k IU from cod liver
vitamin K2-MK4: 5 mg/day
StephenB
Chris,
Congratulations for discovering that connection! I understand now why is my diet high in animal fat and animal produce so much better for me. One of the nice feature is high contents of BOTH vitamins A and D3 at the same time (also K2 but it is hard to get data on that).
Stan (Heretic)
P.S.
I guess, you have also learned some truth about intellectuals and scientists…
8-:)
Chris: Thank for continuing to write and break new ground in the area of D,A,and K. Galen Knight, PhD. discussed the use of topical Red Palm Oil as a rich source of full spectrum Vitamin E at the recent Weston A. Price meeting in S.F. It is also supremely high in beta carotene having 6700 ug retinol equivalent/100 g. (info here:https://www.tropicaltraditions.com/red_palm_oil.htm ). What are your thoughts as to the use of Red Palm Oil in light of the above discussion?
Thank you,
Michael
I have tried supplementing Vit D3 for my daughter who has autism after reading about how many children benefit from it. After a few days of 2000 IU she starts sleeping less and less. I am now wondering whether I should be giving her Vit A at the same time or does she just not need it?
Thanks, Jenene.
Chris:
Thank you for the timely post! I am just getting ready to read the latest issue of “Wise Traditions” which contains your latest cod liver oil article, and will insert a copy of this post into that journal for future reference.
I have been following the vitamin A/D/cod liver oil controversy over the past year or so, and admit I have been “on the fence” about taking HVCLO, and have only done so sporadically over the past 7.5 years. Thanks to you, I am truly convinced now of the importance of adding it to my diet.
For those of you who are leary about eating organ meats, please try nitrate free pastured liver sausage products! US Wellness Meats at: https://www.grasslandbeef.com/StoreFront.bok carries both liverwurst (beef scrap, liver, heart, kidney) and brunsweiger (beef scrap and liver), and my entire (picky) family loves both! Just a single 2 oz slice of the brunsweiger gives roughly 10,000 IU of vitamin A! They are shipped frozen in one pound packages.
Dr. BG and Dan,
Thanks for the props!
While I am willing to consider evidence that synthetic all-trans beta-carotene acts fundamentally differently from natural all-trans beta-carotene, I think the primary factor in the trials where it increased mortality is due to the dose. The same Tufts lab did some compelling research in ferrets showing that at doses obtainable from a diet rich in colorful vegetables, beta-carotene protected against the effect of cigarette smoke, while at doses obtainable only in supplements, beta-carotene was excentrically cleaved to products that induced local deficiencies of retinoic acid (activated vitamin A) in lung tissue, leading to worse precancerous changes itself than caused by cigarette smoke itself. Besides that, huge doses of beta-carotene are outside the range of what is possible on traditional diets, so our default position should be against using mega-doses of carotene. It is easy, by contrast, to obtain pre-formed A in large amounts on a traditional diet by eating liver and organ meats.
Chef Jam,
Yum!
Chris
It's about the Food!
Thank You Chris!
Imagine a grass-fed burger or meat loaf (Nourishing Traditions recipe) topped with grass-fed cheese (just before serving) with your favorite lacto-fermented veggies on the side! Enjoy it at a picnic on a sunny day! A Yummy way for A D K(2)!
What a concept!
Chef Jem
Executive Producer:
"Raw Milk: The Whole Truth"
AKA "The Raw Milk Controversy: Fact & Fiction"
Featuring Mark McAfee of Organic Pastures Dairy
and Dr. Dale Jacobson, DC
Afraid of the idea of drinking raw milk? If so, viewing this video may bring relief!
View four video clips Online at:
https://www.youtube.com/profile_play_list?user=ChefJem33
Over 14,000 total views of the video clips just at YouTube!
Over 35,000 page views at: https://curezone.com/blogs/f.asp?f=1452
Dan,
I wouldn’t worry about the beta carotene studies. As Chris will concur, those were done with Lurotin, a synthetic beta carotene apparently derived from benzene rings (made by BASF in Germany). All the studies were neutral or worse adverse in outcomes, compared with natural beta carotene studies. Similarly negative outcomes have been observed with other synthetic hormones/vitamins…vitamin D2, synthetic Medroxy-provera, oral contraceptives, and other potent hormones.
I’ve reviewed a # of vitamin A studies — all the fat soluble vitamins act synergistically together (with some EPA DHA as well) by heterodimering as nuclear receptors.
https://drbganimalpharm.blogspot.com/search/label/Vitamin%20A
I can’t but help find it all SO fascinating (warning… ‘racy’)
-G
Finally. What I’ve been waiting for 🙂
Thanks Chris — keep up the wonderful job!
Andrew,
I agree you should take them with a meal. I don’t know if there is any advantage to taking both supplements at the same meal, however.
Chris
I take just two supplements, K2 and Cod Liver Oil, and I take them together and I usually try to take them with a meal — and that’s for bioavailability reasons. I’ve just started poking around your blog, Chris; is this something you’ve touched on before?
Not just the vitamins working together once they’re digested, but also for uptake.
Paul,
Yes, that’s strange, and their lit review is basically lifted from my hypothesis paper, but such is life! I’m glad that publishing the paper actually influenced the direction of research, and maybe the Tufts paper will also carry influence and we will start seeing more research taking into account interactions.
Chris
Dan,
You’re welcome! And thank you for your responses.
I’ll be addressing the “increased mortality” in the Cochrane review in the cod liver oil article appearing in the next Wise Traditions. It is a non-finding produced by statistical hocus pocus.
I have not analyzed the other findings in that forum post.
However, you are not part of these populations. You take 2-4000 IU of vitamin D per day. Automatically, you have removed yourself completely from the populations studied in the epidemiological publications, and their findings have no relation to you. You should be getting your vitamin A. Organ meats have been available for as long as humans have been eating animal products.
Chris
Chris,
Thank you for your replies – and your great post!
You are probably right that I don't get enough A. I do eat a lot of eggs, butter, and meat but do not eat organ meat (yet). I have been wary of studies that found negative associations with beta carotene and/or A supplementation (some of them listed in this forum posting: https://www.imminst.org/forum/index.php?s=&showtopic=26533&view=findpost&p=307165).
I want my guide for vitamin intake to be roughly based on what would have been available for the past 100K years. I skip organ meats but do eat a lot of butter (grass-fed), eggs, and muscle meat, along with a fair amount of colored vegetables. I was thinking that my above average K2 intake might make up for some D3-related A deficiency.
Perhaps I am foolishly scared of A, based on some sloppy science. I've been debating this with myself, so I welcome any constructive criticism.
Thanks again!
Great job as always! And too bad the researchers at Tufts didn’t have the common courtesy to keep you apprised of their work. At least a bit of the truth is winning out in the end, though.
Dan,
It occurred to me that I do not have any idea how much vitamin A you are consuming. If you eat organ meats, egg yolks, butter, and vegetables, then I think what you said is good. If you do not eat any liver and do not use other organ meats or cod liver oil, then I doubt you are getting enough vitamin A. The truth is no one has any idea what the ideal intake of vitamin A is once you normalize vitamin D input to 2-4000 IU/day, but I suspect you want at least 1 or 2 times as much A as D in terms of IU. In the absence of organ meats or cod liver oil, many people do not even get the RDA, which is 3,000 IU for adult males — over half the population consumes less, and over a quarter consumes less than half that.
Chris
Bryan,
Thanks!
Chris
Arnoud,
Thanks!
The cod liver oil most likely lowered your vitamin D level by increasing your utilization of vitamin D. The point of having it is to utilize it so that’s not a bad thing.
There is no evidence that I know of supporting a benefit of increasing 25(OH)D from 45 ng/mL to 60 ng/mL, so there is no need to increase your vitamin D dosage.
The test for vitamin K status is undercarboxylated osteocalcin (specifically, not just osteoclacin). Researchers use it routinely but it might be hard to find commercially.
Chris
Kiwi,
No, it’s not that complicated. Sunshine, liver, other organ meats, egg yolks, cheese, fermented foods, and you have the whole shebang. A traditional diet and lifestyle provides what you need.
It becomes complicated if you want to micromanage with supplements and blood tests. That gives us extra security, but humbles us by showing us how little we know.
There is not yet any basis for an RDA of K2 becuase until recently it has been assumed to be of no importance.
MK-4 is in higher doses because it is synthetic and MK-7 is in lower doses because it is naturally isolated from fermented soy. MK-4 is the type of K2 that animal bodies make and has unique functions.
Chris
Very interesting as usual Chris. It’s nice to see theories based on evidence from traditional diets validated by testing. I’m going to continue taking Blue Ice CLO for A and D until my supply runs out. Then I’ll switch to the Green Pastures fermented CLO.
Keep up the good work! I hope you can find a job with an open-minded group that isn’t forced to conform to the world according to big pharma in order to get funding.
Great post! Very interesting to better understand how these vitamins are linked, but it raises questions as to how to best ensure the diet provides adequate levels:
To achieve approximately 60 ng/ml 25OHD3 serum level, I have been taking 8000 i.u. D3 per day (less in Summer). A couple of months ago I started to supplement with cod liver oil, without a change to the D3 supplementation level. The result was that the serum level of 25OHD3 dropped by about 25%. Should I increase the D3 dosage to restore to 60 ng/ml?
Is there any way to tell if one’s K2 level is adequate? Grass fed butter and beef intake should be able to take care of that?
This is getting too complicated.
So those taking D supplements now have to worry about their vitamin A and K2 levels. Getting the 25OH D3 test is no longer enough! And there is still no recommended K2 level, which variety is best, and why the K2-4 and K2-7 supplements have such a large difference in dosage…5mg v 100mcg.
Dan,
That sounds reasonable, although one could simplify it by using high-vitamin cod liver oil including D and just getting less D. 2000-4000 IU D should be from all sources, so less during the summer if you get lots of sunshine.
Chris
Sounds like D3 supplementation should be done along with A and/or K2. Any idea of ratios? Seems like more K2 could mean less A required and conversely more A could mean less K2 required.
Based on a rough comparison to what might have been available to a healthy pre-agriculturalist, I go with 2000-4000IUs daily D3, 1 mg MK-4 (+ 100mcg MK-7) a few times per week, and whatever vitamin A I get from my paleo diet, supplemented with about 1000IU from non-D cod liver oil once a week. Sound reasonable?